Alice Ma, MD, has announced a legacy gift to the UNC hematology fellows, a group she fondly considers her own. Ma’s bequest will go to training in nonmalignant hematology.

Alice Ma, MD, has announced a legacy gift to the UNC hematology fellows, a group she fondly considers her own. Ma’s bequest will go to training in nonmalignant hematology.

A legacy gift is an enduring way to express gratitude and faith in future generations. It can provide future support for special areas of interest, and often, make a gift larger from assets accumulated over a lifetime. For Alice Ma, MD, professor of medicine in the division of hematology and oncology, and director of the hematology fellowship program, a bequest to nonmalignant hematology will sustain fellowship level training.
“I am most passionate about medical student education, but as I considered where I could make the most difference, I decided the fellowship level is where I could have an impact. UNC has done this so well for so long that I knew I wanted to use my estate to continue the tradition in whatever way that it can.”
Need for Nonmalignant Hematology Training
Nearly every specialty has patients with bleeding or clotting disorders or with disorders of blood counts due to non-malignant causes. Medicine recognizes that retention in academic hematology is declining, while a quarter of the nation’s practice-based hematologists are expected to retire in coming years. Ma says adequate training must be maintained in order to treat patients with non-malignant blood disorders.
“If we don’t continue to support fellowship training in nonmalignant hematology, we’re not going to have doctors who are capable of providing nonmalignant hematology care. This is really important because we study the blood that is not cancerous; we take care of patients with clotting and bleeding disorders, with anemia and low platelets. Without our expertise, patients with sickle cell disease don’t get adequate care; without our expertise, patients with hemophilia don’t get subspecialty level care. At the same time, we help patients understand why they have a blood clot, and if a particular condition will be passed to their children. They want to know their risk for having another clot, and why they have to stay on a blood thinner.”
According to Ma, UNC’s level of training is becoming harder to find in a standard hematology-oncology fellowship and is one of only a few places with subspecialty training, supported by UNC’s nationally recognized Hemophilia Center, Sickle Cell Center, and Hemostasis Thrombosis Center, which are central to implementing patient care and research missions.
“We provide subspecialty level care to patients who are undergoing transplants, cardiothoracic surgery and vascular surgery. Consultation requests come from neurosurgery asking how to help the patient who has a brain tumor, who just had a stroke, who needs to be on a blood thinner, or needs to have cardiac surgery but has an allergy to Heparin. These are all consultations that we provide to our surgical colleagues and the patients that they care for. Without our level of care, the care of the surgical patient isn’t optimal.”
Give a Man a Fish or Teach a Man to Fish
The fishing analogy best explains her passion for teaching and how it extends her reach. “When you take care of a patient, you take care of one patient. But when you teach 10 people how to care for the patient, you are taking care of 10 patients because those students will put their learnings into practice.”
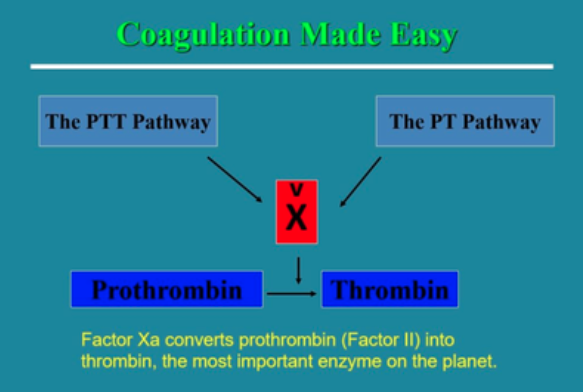
Ma regularly receives emails from people around the world who use her techniques, algorithms, and slide decks for teaching COAG Made Easy. When one student, shadowing a UNC anesthesia professor made the connection that Dr. Ma had taught the professor years before, she was surprised he could still draw the COAG cascade 11 years later.
“If I ever have an obituary someplace important, it will be because I’ve taught in a very simplified way the coagulation cascade to potentially a 100,000 people, and they’ve learned it in a way that even an anesthesiologist can remember 11 years out, even when it’s something that isn’t used every day.”
But one teaching memory will always fill her with pride. It was the time a medical student in her first week saved a patient’s life by noticing a constellation of symptoms she had learned from Dr. Ma.
“She said I heard your voice in my head saying if you see a patient with these symptoms, then you have to think about the diagnosis of thrombotic thrombocytopenic purpura (TTP) and you have to call hematology and start plasma exchange. This brand new third year medical student called us over the 4th of July weekend, and that patient is alive today because of this medical student, and because of what I taught her. That’s as close to immortality as I’m ever going to get.”
To learn about planned giving, contact Director of Development Beth Braxton at beth_braxton@med.unc.edu.