The QI project team led by Jay Lamba, MD, PhD, and Hillary Spangler, MD, is highlighting clinical champions who are frequently using the Deterioration Index Score in EPIC to critically evaluate the health needs of their patients.

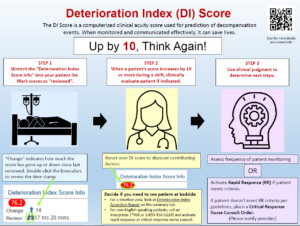
The Deterioration Index (DI) Score in EPIC is a computerized clinical acuity score used for prediction of decompensation events. When monitored and communicated effectively, it can save lives. The MPCU and Rapid Response Team have piloted use of the DI Score during the past year. Learn first-hand how a DI Score “champion” is effectively using this tool.
This week’s feature is of Jennifer MacDonald, a Rapid Response nurse:
Q: What do you find helpful about reviewing a patient’s DI score?
A: The DI score is a useful tool in predicting clinical deterioration and unexpected death. Because the data is generated in real-time and uses values other than just vital signs (such as labs, age, and supplemental oxygen), the tool is a greater predictor of deterioration prior to an actual event than other typical tools (such as MEWS). This allows for earlier treatment and escalation of care, and improved patient outcomes.
Q: How easy or difficult is it for you to review a patient’s DI score?
A: The DI score is very easy to use after wrenching it in through EPIC. There is also a graph which shows the DI score trend for each patient which is helpful in the assessment process. Some patients may have a high baseline DI score (due to a low baseline GCS for example). All members of the Rapid Response Team are trained on the DI score and are a great resource for any questions you might have, whether they are general questions or patient specific.
Q: Do you have an example of where reviewing a patient’s DI score alerted you to the need for an intervention?
A: The DI score identified a patient in the MPCU that was starting to show early signs of sepsis but was in no distress and had stable vital signs. The Rapid Response Team was able to assist with this patient’s care and after a bedside huddle with the primary RN and the physician, a code sepsis was activated. The patient was transferred to the MICU for further escalation of care and closer monitoring. A few days later, they were transferred out to the floor in stable condition. Early identification and treatment of sepsis reduces patient morbidity and mortality.
Please reach out to Jay Lamba MD, PhD, or Hillary Spangler, MD, with questions or suggestions for another DI Score champion. Please also use the tip sheet in this article to learn more about how to use the DI score.