Hospitalized patients with diabetes are dependent on hospital staff to monitor blood glucose, administer medications and deliver meals in a coordinated manner. Inconsistency in the timing of these tasks can increase the risk for hyperglycemia and hypoglycemia. The UNC Department of Medicine’s Value Care Action Group (VCAG) has been working with the division of endocrinology and metabolism to improve glycemic control for hospitalized patients. New services recently introduced are ensuring the safety of patient care and decreasing the length of stay at UNC Medical Center.
“Our department and the hospital realized that we could do a better job of managing blood glucose in our patients,” said Darren DeWalt, VCAG Medical Director and chief of general medicine. “We believed there were some patients who shouldn’t have high glucose, that did, and some who experienced dangerously low glucose, that shouldn’t. This is really a patient safety issue.”
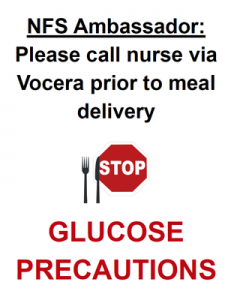
A variety of structural challenges are associated with diabetes care for hospital populations, including providers with varied expertise and inconsistent timing of meal and insulin delivery. Insulin should be delivered as close to meal delivery as possible and that requires careful coordination. A multidisciplinary task force has been working to solve this problem. This team includes nursing, physician, advanced practice providers and nutrition services and their first initiative “Glucose Precautions” has rolled out at UNC medical center. With this project in place, nursing and food services now work in concert to ensure insulin is administered at the proper time in relation to meal consumption.
A team of advanced practice providers, led by Morgan Jones, MD, assistant professor in the division of endocrinology and metabolism, are also providing dedicated support for patients with diabetes at UNC Medical Center. With expertise in inpatient glucose management, this care team is able to co-manage patients with diabetes and provide important transitions from inpatient to outpatient diabetes care. This is achieved by not only providing important medication recommendations at the time of discharge, but also through a virtual care follow up clinic after discharge with the Diabetes Care Team.
New Safety Guards 
Additional safety guards have been implemented in the environment. Signs are placed on patient doors that say “Glucose Precautions” which identifies people at risk of hyper or hypoglycemia. A table tent is delivered with each patient meal that says “Glucose Precautions” and recommends patients remind their nurse to bring insulin with their meal. Food services employees that deliver trays now send a message to the nurse of all patients with “Glucose Precautions” ensuring they are aware the patient is about to eat and they will need their insulin.
Since the inception of the Diabetes Care Team in July, 2019, led by April Goley, FNP-C, and Bonnie Alexander, PA-C, glycemia improved at UNC Medical Center, as efforts continued through a transition to “virtual care” due to the COVID-19 pandemic, without detriment to patient care. In fact, Jones and the team published the results May 29, 2020, in Diabetes Technology and Therapeutics and have recognized endless possibilities for expansion throughout the UNC Health system.
“Initially, the team consisted of one nurse practitioner, April Goley, and it was through her hard work that we’ve been able to show the value of dedicated resources,” said Scott Keller who directs business development for the department. “This effort will provide much of the groundwork for a system-wide project focused on improved blood sugar control at all UNC Health sites. We also thank Dr. Jones for all of his efforts, and the example he has set for value improvement throughout the department.”
Hypoglycemia Committee
This diabetes improvement directive is also focused on a thorough review of hypoglycemic events, a major and preventable cause of morbidity and mortality in hospital settings. UNC Medical Center’s Hypoglycemia Committee identifies systemic issues that cause inpatients to experience low blood sugar and the review considers practice protocols, prescribing patterns and education of providers and nursing staff. Now, the Committee will assume a more data-driven approach to identifying problems and solutions. The change will enhance existing efforts to decrease hypoglycemic events that may be preventable.
Value-Care Action Group
This glucose management project is one of many Value Care Action Group improvement efforts taken up by the UNC Department of Medicine. Ron Falk, MD, chair of the department created the group and appointed champions in each medicine division, encouraging the review of current practices that look for improvements for high-value outcomes in healthcare. High-value is defined by the quality of patient-centered care achieved per unit of cost. Scott Keller is the director of business development keeping the team focused on value-oriented care models. Darren DeWalt, MD, serves as medical director for the team and helps define the projects. John Vargas is the project manager.