Mara Buchbinder, PhD, professor of social medicine, and colleagues at the UNC School of Medicine and Harvard University surveyed obstetrician-gynecologists in 13 states with functional abortion bans to document the impacts on healthcare staff.
CHAPEL HILL, NC – UNC School of Medicine researchers and colleagues have documented the perceived effects on physicians in the wake of the Dobbs v. Jackson Women’s Health Organization U.S. Supreme Court decision of June 22, 2022, after which 16 states functionally banned abortion with only limited exceptions based maternal health, rape, incest, and fatal fetal anomalies. Five other states have similar legislation pending.
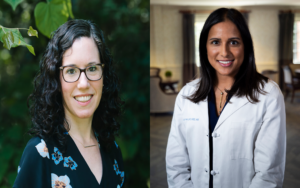
The study, led by Erika L. Sabbath, ScD, at the Harvard T.H. Chan Center for Work, Health and Wellbeing, and Mara Buchbinder, PhD, professor of social medicine at the UNC School of Medicine, was published in JAMA Network Open. Kavita Arora, MD, associate professor and division director for general obstetrics, gynecology, and midwifery at the UNC School of Medicine, was also a co-author. The team interviewed 54 obstetrician-gynecologists in 13 states with the most severe abortion restrictions. The authors of the JAMA paper found that obstetrician-gynecologists reported “deep and pervasive impacts of state laws, with implications for workforce sustainability, physician health, and patient outcomes.”
The researchers documented clinical impacts, such as delayed care or an inability to provide care due to nebulous legal interpretations of state law by their own healthcare organization administration. One physician told the researchers, in relation to providing patient care, “The way our legal teams interpret [the law], until [patients] became septic or started hemorrhaging, we couldn’t proceed. It puts women in a very challenging, risky position. [According to the law], is a 5% risk of death enough? Does it take 20%? Does it take 50%? What is enough legally. And the legal people seem to have a different definition that also just feels horrible to say: until [the patient] is at a greater than likely chance of dying, you can’t make a decision as a doctor.”
The researchers documented counseling restrictions and the inability to provide care even if there were no counseling restrictions. They also reported on the moral distress of obstetrician-gynecologists who could not follow clinical standards due to legal constraints. The authors wrote, “When describing their moral distress over such encounters, [participants] used words like muzzled, handcuffed, and straitjacketed. One said, ‘I know what the right thing is to do for my patients, but I am carrying this legal worry and worried about what could happen to my family at the same time.’”
About 87% of study participants reported worries related to practicing in an uncertain legal climate. Fears centered on potential for criminal prosecution, loss of medical license, loss of income, and incarceration.
The researchers reported that 11% of physicians interviewed had moved their practices to other states after the Dobbs decision. About 60% had considered leaving their state but such a move was not possible for them due to personal ties to their communities. In contrast, the researchers say some obstetrician-gynecologists are committed to staying in their communities. One said, “I’ve thought so many times about leaving, but I’m only one of three people, really, in this state who can take care of a patient who his possibly dying from their pregnancy. And that makes me want to stay.”
The researchers also reported that 70% of participants reported mental health issues, such as anxiety and depression, due to the new and often confusing legal restrictions. Some have had to seek mental health counselling in part due to the lack of legal clarity surrounding the care they are allowed to provide to pregnant women with health complications. One such obstetrician-gynecologist said she had never needed counseling prior to this, not even after deploying to Iraq, leaving a 15-month-old baby at home with her husband, to practice medicine in a warzone.
The authors say their findings “suggest the need of healthcare organizations to invest in efforts to support, attract, and retain OB-GYNs in restrictive states, and to protect physicians’ own health and that of their patients.”
This research was supported by the Making a Difference grant from the Greenwall Foundation.