Researchers in the lab of Jean Cook, PhD, chair and professor in the Department of Biochemistry and Biophysics, have identified the cellular processes that occur when you take a cancer drug meant to stop rapid cell growth in tumors.
Cancer cells can hijack cell cycles to exponentially increase their numbers, a process called proliferation. Cancer drugs can stop the growth of cancer cells by jumpstarting a complex chain of genetic and cellular events. But often, this story is more complex, involving treatments that don’t work as well as had been hoped.
New research from the lab of Jean Cook, PhD, chair and professor in the Department of Biochemistry and Biophysics, suggests that a particular enzyme is essential for halting cancer cell proliferation, specifically when patients are being administered anticancer drugs. But this enzyme’s function is not equal in all of us. Cook’s lab also figured out interesting details about how cancer cells can escape therapy designed to stop them.
Their findings, published in Proceedings of the National Academy of Sciences, offer more insights for drug developers to consider in the battle against cancers.
Cells can turn genes “on” and “off” to control the expression of certain proteins. Some proteins have the job of maintaining accurate and effective cell division, much like musicians in an orchestra under control of a conductor. Cells have the ability to “shut off” the controls of these regulatory proteins (i.e., remove the conductor), and this allows the cells to divide without restraint and replicate DNA for newly formed cells.
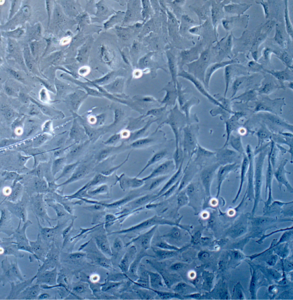
To isolate and home in on the role protein degradation plays in stopping cell growth, Cook and her graduate student Brandon Mouery, first treated cultured human cells with palbociclib, a metastatic breast cancer drug that targets cell proliferation. By using microscopy, flow cytometry, and proteomics, the researchers discovered that the enzyme APC/C, which normally targets proteins for degradation to regulate the cell cycle, helps maintain the positive effects of palbociclib.
This finding suggests doctors could leverage APC/C levels in cancerous tumors to predict how well patients may respond to palbociclib and other anticancer drugs in the same class. For example, reduced APC/C activity may indicate that a patient may have a poor reaction to treatment or could be at an increased risk of relapse.
Cook and Mouery also found that cancerous and non-cancerous cells can escape drug-induced proliferation arrest and that the escapee cells have a difficult time replicating DNA on their own. A potential explanation is that they “pass off” their DNA replication duties to proteins that initiate cell division towards the end of the cell cycle. The observations suggest that cells have alternate molecular pathways that they can use to spur uncontrolled cell growth.

“Cell proliferation has been intensively studied for decades, yet we can still be surprised,” said Cook, who is also a member of the UNC Lineberger Comprehensive Cancer Center. “In this instance, we discovered cells can run their cell cycle with an upside-down order of events. Sometimes our textbook understanding is still quite incomplete, so we need to keep an open mind and continually challenge paradigms.”
The new findings could lead to new interventions that can provide long-lasting proliferation arrest effects. By combining their knowledge of this newfound escape route with cancer-associated DNA replication errors, they could pave new ways to force cancer cells to grow in a “self-destructive” way.
Media contact: Kendall Daniels, Communications Specialist, UNC Health | UNC School of Medicine