Washington, N.C man with squamous cell carcinoma of the tongue experiences positive life-changing results after participating in an induction therapy clinical trial at the UNC School of Medicine.
CHAPEL HILL, N.C. – In the summer of 2018, Vance Aldrich Bell III of Washington, North Carolina was in a routine dental checkup when his dentist found a suspicious spot on his tongue. A biopsy revealed that the spot was benign, so Bell was asked to keep an eye on it.
Three years later, his tongue started to feel strange. It began to swell to the size of a lime. He started to have trouble speaking and swallowing. He rushed to urgent care, then to a local ENT physician, where another biopsy of his tongue was taken. Not soon after, he was diagnosed with squamous cell carcinoma – a cancer that develops in skin cells and the linings of the digestive and respiratory tracts – which had spread to nearby lymph nodes in the neck.
“I just remember kind of going blank and not really hearing much beyond ‘cancer,’” said Bell. “I don’t really remember feeling much – it just takes the wind out of your sails, so to speak. It was like a gut punch.”
Bell knew that he would eventually need surgery to remove the cancer from his tongue. His friends had referred him to a handful of specialists, but he eventually chose Wendell G. Yarbrough, MD, MMHC, FACS, an experienced head and neck surgeon at UNC Hospitals.

“I think he had close to a 5 or 6 cm tumor,” said Yarbrough, who is the Thomas J. Dark Distinguished Professor of Otolaryngology/Head and Neck Surgery in the UNC School of Medicine. “With a tumor of that size, you can imagine that a lot of his tongue would have to be excised to remove the tumor, and then, after that, people frequently get radiation or chemotherapy, and we take out lymph nodes in the neck.”
But Yarbrough had something else in mind. He knew of a clinical trial for induction therapy that was still accepting patients. Induction therapy is a short course of medicines, in this case two chemotherapy drugs given at low dose plus immunotherapy.
The goal of the clinical trial, led by Jared Weiss, MD, an oncologist at the UNC Lineberger Comprehensive Cancer Center, was to shrink the tumor down as much as possible prior to surgery, in the hopes that it would make the surgery more effective and less severe. More importantly, it could reduce one’s chances of needing radiation after the surgery, which could lead to debilitating side effects down the line, such as necrosis of the jaw, dental issues, dry mouth, speech and swallowing problems, and even aspiration – when food enters the airway where it can get lodged.
“The trial is only six weeks of low dose weekly therapy, and, critically, it’s not leading to permanent harm to quality of life,” said Weiss, who is a professor of medicine and the section Chief of Thoracic and Head/Neck Oncology in the Department of Medicine. “The goal here was to not only cure more patients, but to improve their long-term quality of life by either omitting radiation therapy entirely or by limiting the field size in those who had some response.”
Bell was introduced to Weiss to learn more about the clinical trial. For the first time since his trip to the dentist, he realized that he didn’t feel like a number and felt genuinely cared for by Weiss, Yarbrough, and the other medical staff at UNC.

“Early on, everyone else’s answer or plan was surgery and radiation,” said Bell. “Dr. Yarbrough was receptive and shared the idea of a potential trial and Dr. Weiss was very personable, intelligent, and able to ‘dumb down’ really difficult concepts for me. Finding people that genuinely care about you puts you in a better place than feeling like you’re just a number.”
After much deliberation and prayer, Bell decided that he would participate in the trial. He received low dose therapy of carboplatin, nano-albumin bound paclitaxel, and durvalumab over the course of six weeks. His response was remarkable. His tumor had shrunk from the 5 cm to 1.5 cm, or about the size of a peanut.
Yarbrough and his surgical team performed a smaller surgery than they had originally anticipated because of the positive response. They only needed to remove less than half of Bell’s tongue. They also discovered that his lymph nodes were negative at the time of surgery, which may have also been a result of the induction therapy.
Catherine J. Lumley, MD, assistant professor in the Department of Otolaryngology, was then tasked with reconstructing his tongue. She removed a portion of Bell’s left wrist – skin, muscle, arteries, and all – and reconstructed the second half of his tongue. She then removed all the lymph nodes in Bell’s neck to excise any cancer that may be lurking around. All in all, Bell’s response was so strong that he was able to circumvent radiation altogether.
“I won’t say I’m 100% the same as I was pre-surgery,” said Bell. “Obviously, my tongue is different and I have a scars on my neck and arm that others don’t, but I don’t have any limitations to speak of. There are some things that may be harder to do now, but I feel like I’m very blessed to have landed at UNC Health and receive such a high level of care.”
Bell is just one of many trial participants who have had success with this trial. Some participants have had a “complete response” to the induction therapy, meaning that there is no tumor left, even under the microscope. It brings to question if this could become a new treatment standard for patients with squamous cell carcinoma.
“We’ve had a few people who’ve had complete responses after induction therapy,” said Yarbrough. “I think this is going to be part of our treatment in the future. The real question for us is, which patients should get induction therapy? Who’s going to respond to this therapy? And who’s not going to respond?”
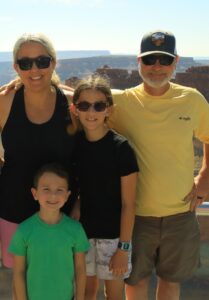
Bell is now two years in remission. Bell is still incredibly grateful for his wife Sara, who was instrumental in supporting him spiritually, physically, and mentally by taking care of his wounds and maintaining a positive outlook throughout his medical journey. He also frequently thinks back to the profoundly personal patient experience that he had at UNC.
“It isn’t just a medical appointment when I visit UNC Health,” said Bell. “Dr. Yarbrough and I talk about UNC basketball. Dr. Weiss and I talk about poker. I got to know these people and they got to know me. For me, it was important to find the right team that genuinely cares – they helped me recognize that although cancer is bad, it isn’t the end. They are just good people and they’re a great team.”
To learn more about Mr. Bell and his care team, watch this Leading the Way video.
Media contact: Kendall Daniels, Communications Specialist, UNC Health | UNC School of Medicine